medical Necessity and revision
Quick question: what criteria are most insurance companies looking for,for one to qualify for a revisional bariatric surgery? I know the band has their criteion. but what are those for Bypasser to DS revision? I call the insurer who states medical necessity. but that is so vague. I look up a few insurers on google but insurers seem to have difference of opionion. What is out there or more specifically for EMPIRE governmental plan does anyone know?
Medical necessity can be defined as still being obese and having comorbidities. It can also be for mechanical failure - things like a dirupted staple line, a stretched stoma, etc. I had my revision because the ring around my stoma (a little something extra some docs used to do) caused constant vomiting and esophageal erosion. They granted it based on that.
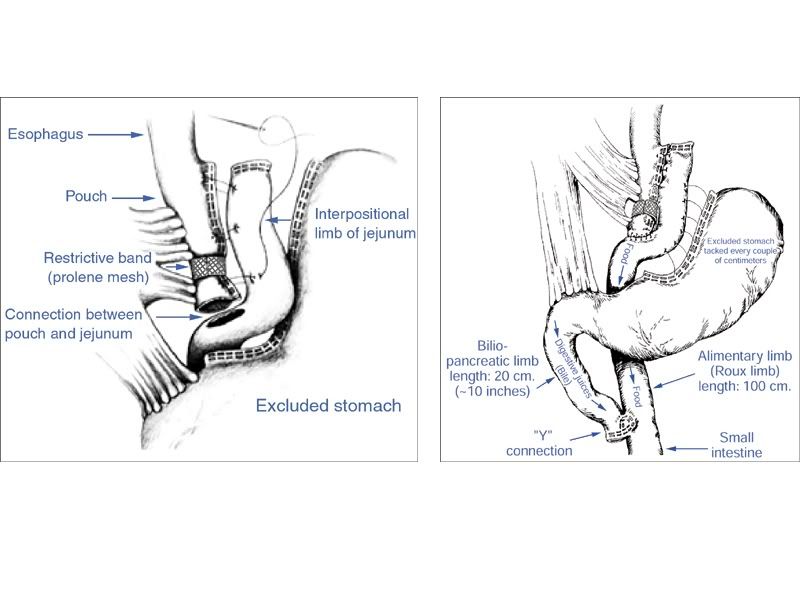
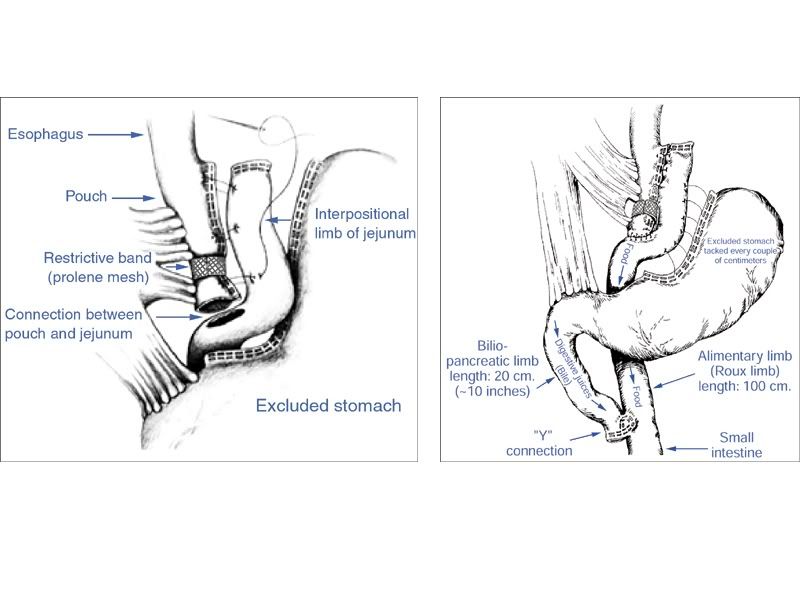
Nope, no fobi pouch. Dr. Kamelgard followed Dr. Capella's method of including a prolene mesh band around the stoma to create a combination RNY with VBG. From his files:
A picture of Dr. Kamelgard explaining this at a support group meeting:
This was done to keep the stoma from stretching, to prevent regain. Didn't work. Lots of people regained because the only thing they could keep down were soft foods like carbs.
A picture of Dr. Kamelgard explaining this at a support group meeting:
This was done to keep the stoma from stretching, to prevent regain. Didn't work. Lots of people regained because the only thing they could keep down were soft foods like carbs.



