Lurkers, Learn Here About Your Pyloric Valve (informative input from post ops welcome)
I am going to copy and paste some info, basically because others can explain it far better than my own incoherent ramblings.
http://www.britannica.com/EBchecked/topic/484656/pylorus?anchor=ref237588
pylorus,
cone-shaped constriction in the gastrointestinal tract that demarcates the end of the stomach and the beginning of the small intestine. The main functions of the pylorus are to prevent intestinal contents from reentering the stomach when the small intestine contracts and to limit the passage of large food particles or undigested material into the intestine.
The internal surface of the pylorus is covered with a mucous-membrane lining that secretes gastric juices. Beneath the lining, circular muscletissue allows the pyloric sphincter to open or close, permitting food to pass or be retained.
A normal functioning stomach.....
http://www.healthhype.com/normal-gastric-stomach-emptying.html
What is gastric emptying?
Gastric emptying is the process by which the stomach empties its contents into the duodenum of the small intestine for further digestion of food and absorption of nutrients. While this may seem like a simple process, it is carefully coordinated so as not to overwhelm the duodenum with large amounts of partially digested food mixed with the acidic gastric secretions, which is collectively known as chyme.
Ask a Doctor Online Now.
How does gastric emptying work?
The stomach is a muscular, hollow organ. When food enters the stomach, it is churned by the stomach contractions (peristalsis) with gastric secretions (refer to Gastric Acid Secretion) and this allows for both mechanical and chemical digestion. Most of this churning occurs within the body of the stomach where the muscle contractions are weak.
The contractions lower down the stomach, near the pylorus, are more intense. This pushes the more fluid chyme through the pylorus while undigested food particles are forced higher up into the stomach for further breakdown. These stronger peristaltic waves that occur near the pylorus propel the fluid chyme through the pylorus into the duodenum in a pump-like action. This is referred to as the ‘pyloric pump‘.
The distal part of pylorus has a thick muscular wall arranged in a circular manner which remains contracted in a normal state. This is known as the pyloric sphincter. Even though it is contracted, the sphincter is not totally closed and there is gap which allows fluids like water or chyme to move through into the duodenum but prevents the movement of larger food particles.
What promotes or inhibits gastric emptying?
The vagus nerve is mainly responsible for parasympathetic stimulation to the stomach. This increases peristalsis and opens the pyloric sphincter. Sympathetic stimulation via the celiac plexus inhibits peristalsis and the opening of the sphincter. This is influenced by brain stem as well as stimuli from the sensory nerve endings in the gastric epithelium. Refer to Stomach Nerves for more information on the stomach nerve supply.
.jpg)
And here is an image of the VSG, which is also the restrictive component of the BPD/DS. Note the Pylorus has been left in tact.
www.obesityhelp.com
Duodenal Switch (DS) |
|
|
|
http://www.mayoclinic.com/health/dumping-syndrome/DS00715/DSECTION=causes
Causes
By Mayo Clinic staff |
Stomach and pyloric valve |
In dumping syndrome, food and gastric juices from your stomach move to your small intestine in an unregulated, abnormally fast manner. This accelerated process is most often related to changes in your stomach associated with surgery. For example, when the opening (pylorus) between your stomach and the first portion of the small intestine (duodenum) has been damaged or removed during an operation, dumping syndrome may develop.
Dumping syndrome may occur at least mildly in one-quarter to one-half of people who have had gastric bypass surgery. It develops most commonly within weeks after surgery, or as soon as you return to your normal diet. The more stomach removed or bypassed, the more likely that the condition will be severe. It sometimes becomes a chronic disorder.
Gastrointestinal hormones also are believed to play a role in this rapid dumping process.
http://emedicine.medscape.com/article/173594-overview
Background
The stomach serves as the receptive and storage site of ingested food. The primary functions of the stomach are to act as a reservoir, to initiate the digestive process, and to release its contents downstream into the duodenum in a controlled fashion. The capacity of the stomach in adults is approximately 1.5-2 liters, and its location in the abdomen allows for considerable distensibility. Gastric motility is regulated by the enteric nervous system, which is influenced by extrinsic innervation and by circulating hormones. Alterations in gastric anatomy after surgery or interference in its extrinsic innervation (vagotomy) may have profound effects on gastric emptying. These effects, for convenience, have been termed postgastrectomy syndromes.
Postgastrectomy syndromes include small capacity, dumping, bile gastritis, afferent loop syndrome, efferent loop syndrome, anemia, and metabolic bone disease. Postgastrectomy syndromes are iatrogenic conditions which may arise from partial gastrectomies, independent of whether the gastric surgery was initially done for peptic ulcer disease, cancer, or for weight loss (bariatric). The surgical procedures include Billroth-I, Billroth-II, and Roux-en-Y.1
Pathophysiology
Dumping is the effect of altered gastric reservoir function, and abdominal postoperative gastric motor function.2The early dumping syndrome and reflux gastritis are less frequent when segmented gastrectomy rather than distal gastrectomy is performed for early gastric cancer.3 In persons with long segment Barrett esophagus treated with a truncal vagotomy, partial gastrectomy, plus Roux-en-Y gastrojejunostomy, 41% developed dumping within the first 6 months after surgery, but severe dumping is rare (5% of cases).4
The dumping syndrome occurs in 45% of persons who are malnourished and who have had a partial or complete gastrectomy.5 The late dumping syndrome is suspected in the person who has symptoms of hypoglycemia in the setting of previous gastric surgery, and this late dumping can be proven with an oral glucose tolerance test (hyperinsulinemic hypoglycemia), as well as gastric emptying scintigraphy that shows the abnormal pattern of initially delayed and then accelerated gastric emptying.6
Clinically significant dumping syndrome occurs in approximately 10% of patients after any type of gastric surgery. Dumping syndrome has characteristic alimentary and systemic manifestations. It is the most common and often disabling postprandial syndrome observed after a variety of gastric surgical procedures, such as vagotomy, pyloroplasty, gastrojejunostomy, and laparoscopic Nissan fundoplication. Dumping syndrome can be separated into early and late forms, depending on the occurrence of symptoms in relation to the time elapsed after a meal. Both forms occur because of rapid delivery of large amounts of osmotically active solids and liquids into the duodenum. Dumping syndrome is the direct result of alterations in the storage function of the stomach and/or the pyloric emptying mechanism.
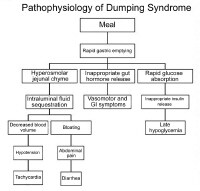
Pathophysiology of dumping syndrome.
The accommodation response and the phasic contractility of the stomach in response to distention are abolished after vagotomy or partial gastric resection.7 This probably accounts for the immediate transfer of ingested contents into the duodenum. Hertz made the association between postprandial symptoms and gastroenterostomy in 1913.8 Hertz stated that the condition was due to "too rapid drainage of the stomach." Mix first used the term "dumping" in 1922 after observing radiographically the presence of rapid gastric emptying in patients with vasomotor and gastrointestinal (GI) symptoms.
The severity of dumping syndrome is proportional to the rate of gastric emptying. Postprandially, the function of the body of the stomach is to store food and to allow the initial chemical digestion by acid and proteases before transferring food to the gastric antrum. In the antrum, high-amplitude contractions triturate the solids, reducing the particle size to 1-2 mm. Once solids have been reduced to this desired size, they are able to pass through the pylorus. An intact pylorus prevents the passage of larger particles into the duodenum. Gastric emptying is controlled by fundic tone, antropyloric mechanisms, and duodenal feedback. Gastric surgery alters each of these mechanisms in several ways.
Gastric resection reduces the fundic reservoir, thereby reducing the stomach's receptiveness (accommodation) to a meal. Vagotomy increases gastric tone, similarly limiting accommodation. An operation in which the pylorus is removed, bypassed, or destroyed increases the rate of gastric emptying. Duodenal feedback inhibition of gastric emptying is lost after a bypass procedure, such as gastrojejunostomy. Accelerated gastric emptying of liquids is a characteristic feature and a critical step in the pathogenesis of dumping syndrome. Gastric mucosal function is altered by surgery, and acid and enzymatic secretions are decreased. Also, hormonal secretions that sustain the gastric phase of digestion are affected adversely. All these factors interplay in the pathophysiology of dumping syndrome.
I didn't find OH until I was recovering from surgery. I love my RNY but I fear not being able to retain what I have worked so hard for. Keep educating us!!
 Connie
Connie People need to realize that doctors are business folk and they are selling something (bariatric surgeons anyway). Go in with both eyes open folks. They don't give a **** about you for real, obesity is their money maker.
Know how a surgery will change your body. Lapband changes your body permanently, so do all the others. Don't be fooled, know what you're getting.
CW= 145 ***GOAL REACHED on Christmas Day 2010****
GW=145
5'6" BMI= 23
LapBand 3/2006 to Revision DS 12/2009
Get the FACTS about the Duodenal Switch at www.DSFACTS.com or http://www.duodenalswitch.com/
Extended Tummy Tuck, BL/BA scheduled for 11/18/11 Dr. Larry Lickstein
on 2/15/11 12:25 pm
"Our ultimate freedom is the right and power to decide how anybody or anything outside ourselves will affect us." Stephen Covey
Don't litter! Spay or neuter your pet
My second surgeon, like night and day. Dr. Sudan wanted to hear my story. He wanted to know why I wanted DS over other surgeries and in end the end pyloric preservation was just as much a concern of his as it was mine.
My RNY doctor never really explained that some of the negative side effects of RNY centered around cutting away the pylorus. I just want people to know what it is and how it functions, to use in their own research. Nobody ever told me, I had to find out on my own.
I'm not a sheeple. So their aftercare is fairly worthless to me.
Liz
Duodenal Switch (Lap) 01-24-11 | Surgeon: Stephen Boyce | High weight: 250 in 2002 | Surgery weight: 203 | Lowest weight: 121 | Current weight: 135 | Goal weight: 135
My comment was in general about some doctors and their lack of care for us. I have had awesome doctors but more often than not, they were awful! Now, my docs are all great....hmmmmm? Wonder what the difference is? Connie

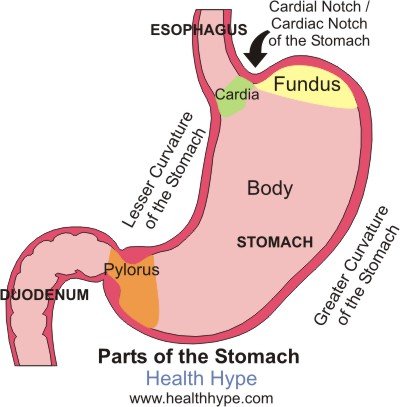
 An improvement of the BPD (it is also referred to as “BPD/DS"). Here again, there is a significant malabsorptive component which acts to maintain weight loss long term. The patient must be closely monitored to guard against severe nutritional deficiencies. This procedure, unlike the BPD, keeps the pyloric valve intact. That is the main difference between the BPD and the DS.
An improvement of the BPD (it is also referred to as “BPD/DS"). Here again, there is a significant malabsorptive component which acts to maintain weight loss long term. The patient must be closely monitored to guard against severe nutritional deficiencies. This procedure, unlike the BPD, keeps the pyloric valve intact. That is the main difference between the BPD and the DS.

