Okay, I'm clueless, what is DS...I made need a revision and .....
The small stomach that is left intact with the DS will stretch back to a normal (but smaller) sized stomach with time. Opponents of the DS argue that the removal of the stomach is a bad thing. In fact, it is not a bad thing--the blind pouch left off to the side with the RNY is a bad thing. This blind pouch is inaccessible to endoscopy evaluation, thus you cannot be diagnosed in the future with problems such as ulcers or tumors, etc. This is why RNYers cannot take NSAIDs because of the potential for ulcer formation in the blind pouch. DS patients can take NSAIDS with no problem.
It is the malabsorptive portion of the DS that results in the superior long-term excess weight lost (around 85%). More of the intestines are bypassed in the DS than the RNY resulting in more malABSORBTION of calories, but NOT more malNURTRITION because of the superior digestion of a fully functional stomach instead of a man-made pouch.
Although the size of the stomach is reduced with this procedure, the
pyloric valve of the stomach, which controls the emptying of food
from the stomach into the intestines, remains in tact. With the RNY
there is a man-made pouch which allows food to pass freely through
the man-made "stoma" from the pouch into the intestines
resulting in dumping syndrome (a potentially-dangerous, sudden jump
in blood-sugar level caused by undigested food entering the
intestines), stomal ulcers, and vitamin deficiency due to poor
digestion. The malabsorption component of the Duodenal Switch as
relates to CALORIES from fat is GREATER than with the RNY because
more of the intestine is bypassed. The DS retains a normal,
functioning stomach with access to all the digestive juices, etc.,
rather than a man-made pouch.
Long-term excess weight lost and kept off is better with the DS.
After the “honeymoon” period of the first year or two of rapid weight
loss ends, 20% (or 1 in 5) of post-op RNY patients gain back 50% or more of
the excess weight lost. The DS combines both restrictive and
malabsorptive elements to achieve and maintain the best reported
percentage of excess weight loss, 80-85% with little or no regain.
The DS surgery without gastric reduction has been
performed on non-obese, diabetic patients since 1997 and is
increasing in popularity in Europe as an IMMEDIATE CURE for type II
diabetes. Latest studies on this technique report a 98% rate of cure.
This is attributed in theory to the malabsorption component of the
DS. The RNY does not cure diabetes. It only puts it in remission, and
the disease oftentimes comes back in two or three years--even if the
patient maintains most of their weight loss. It seems even a small
weight gain long-term (which is the norm) will cause diabetes
relapse.
Here's a list of careful studies which demonstrate the efficacy and safety of the DS procedure:
· Results of Ten Years or More Post-DS by Dr. Douglas S. Hess (128-138) (preprint which was recently published as "The Biliopancreatic Diversion with the Duodenal Switch: Results Beyond 10 Years," Hess, Douglas S.; Hess, Douglas W.; Oakley, Richard S.; Obesity Surgery, March 2005, vol. 15, no. 3, pp. 408-416(9) which concludes, “...it can be seen that the DS procedure is a safe and extremely effective procedure for weight loss, in fact more effective long-term than the more commonly used Roux-en-Y gastric bypass surgery. It is essentially a cure for Type II diabetes. Other long-term studies have shown little or no serious or irremediable nutritional sequellae, contrary to frequently expressed—but unsubstantiated—concerns. It has been successfully performed in our practice for over ten years, and for several years longer in other practices, and has in our opinion become, if not the “gold standard,” the “platinum standard” for bariatric surgery. It is certainly no longer considered an experimental or investigational procedure, either by the American Society for Bariatric Surgery (ASBS) or by the surgeons who perform it” .
· The Duodenal Switch Operation for the Treatment of Morbid Obesity by Gary J. Anthone, MD; Reginald V. N. Lord, MD; Tom R. DeMeester, MD; Peter F. Crookes, MD (188-189). This study included 701 patients who underwent longitudinal gastrectomy with duodenal switch operation. The mean loss of excess body weight exceeded 65% at five or more years. Perioperative mortality was 1.4% and morbidity was 2.9%. The study concludes, “the ...duodenal switch is a safe and effective primary procedure for the treatment of morbid obesity. It has the advantage of allowing acceptable alimentation with a minimum of side effects while producing and maintaining significant weight loss. These results are achieved without developing significant dietary restrictions or clinical metabolic or nutritional complications” .
· Duodenal Switch: an Effective Therapy for Morbid Obesity—Intermediate Results (190-194): Published in 2001 in Obesity Surgery, this article reflects the intermediate results of Dr. Baltasar’s DS study which has been ongoing and reported for several years. Dr. A. Baltasar is chief of Surgical Service; Surgical Staff; Surgical Resident; at Virgen de los Lirios Hospital, Alcoy, Alicante, Spain: 125 patients were in the study from 1994 to 2000. No patients were lost to follow-up. Dr. Baltasar reports the DS as “the most effective operation to lose weight” (193). He cites a major benefit of the surgery as patient quality of life in that patients can eat virtually all foods and do not suffer the major restriction of the restrictive Roux-en-Y gastric bypass procedure. The weight loss has been consistent with the other studies.
· Biliopancreatic Diversion with a Duodenal Switch (195-216). In 1998, Dr. Hess of Bowling Green, Ohio, published a 10-year follow-up report on the first 440 patients to undergo his BPD/DS proceudre in Obesity Surgery, the leading journal addressing issues related to surgical treatment of morbid obesityh. Generally considered the “father” of the DS operation, having integrated the Scopinary BPD with Dr. DeMeester’s DS procedure, Hess reported his results on 440 patients. The paper outlines many advantages to the DS procedure and states, “this method of surgery has been the most successful for patient weight loss that we have used so far” (216).
· 1998 Scopinaro Report (217-236): The BPD procedure (without the duodenal switch), on which the BPD/DS is based, was first performed in 1976 by Dr. Nicola Scopinaro of Italy. In 1998, Dr. Scopinaro published a 21-year follow-up report on a series of 2241 BPD patients. This report concludes that the BPD is “the most effective procedure for the surgical treatment of obesity” (233).
· Biliopancreatic Diversion with a New Type of Gastrectomy (172): In 1993, Dr. Picard Marceau of Laval, Canada, published a report on the benefits of the BDP/DS procedure over the unmodified BPD. This report confirms that the DS procedure eliminates or greatly minimizes most negative side effects of the original BPD (172).
· Nutritional Markers following Duodenal Switch for Morbid Obesity (567-574): This study was published in the 2004 Jan:14(1):84-90 issue of Obesity Surgery and concludes the the DS “is not associated with broad nutritional deficiencies. Annual laboratory studies, which are required following any type of bariatric operation, appear to be sufficient to identify unfavorable trends. In selected patients, additional iron and calcium supplementation are effective when indicated” (568). This study was submitted to dispute the claim made in BC/BS’s policy that “BPD with or without Duodenal Switch has malabsorptive properties and eventual metabolic complications have been demonstrated” (547). This assertion is simply not true any more for the DS than for the RNY which BC/BS readily covers.
· Comparison of Nutritional Deficiencies after Rouxen-Y Gastric Bypass and after Biliopancreatic Diversion with Roux-en-Y Gastric Bypass (Abstract of a study published in Obesity Surgery in August 2002) (576): This study concludes that there is no significant difference in the incidence of deficiency of the nutritional parameters studied, except for ferritin (37.7% low ferritin levels after RYGBP vs. 15.2% after BPD, P=0.0294). This study was submitted as this was the only DS-related study listed as a reference (263) by the Anthem Blue Cross Blue Shield policy (253-269), which deems there is sufficient evidence to support the BPB/DS (254).
Among the advances of the DS procedure is the absence of dumping syndrome (a potentially-dangerous, sudden jump in blood-sugar level caused by undigested food entering the intestines through a man-made opening), stomal ulcers, and vitamin deficiency commonly seen with the Roux-en-Y (RNY), the compulsory procedure covered by BC/BS of AL (165, 170-237, 267, 559). With the DS, the patient retains their naturally functioning stomach (although the volume is reduced) along with the pyloric valve or natural exit from the stomach to the intestines rather than a problematic, man-made “pouch” as with the RNY (165). Other advantages of the DS are better sustained long-term excess weight loss, a 98 percent cure (181, 183) rate for type II diabetics and ability to take NSAIDs, non-steroidal anti-inflammatory medications. Another advantage still is that the entire stomach and duodenum can be visualized by endoscopy, unlike the RNY which divides the stomach into an upper and lower pouch, the lower of which cannot be visualized endoscopically (165).
Among the advances of the DS procedure are the following:
· Rarity of dumping syndrome (a potentially-dangerous, sudden jump in blood-sugar level caused by undigested food entering the intestines through a man-made opening), commonly seen with the Roux-en-Y (RNY).
· NO stomal ulcers commonly seen with the Roux-en-Y (RNY).
· The DS patient retains their naturally functioning stomach (although the volume is reduced) along with the pyloric valve or natural exit from the stomach to the intestines rather than a problematic, man-made “pouch” as with the RNY.
· Better sustained long-term excess weight loss and, unlike the RNY, a low failure rate.
· A 98 percent cure rate for type II diabetes.
· The ability to take NSAIDs, non-steroidal anti-inflammatory medications.
· The entire stomach and duodenum can be visualized by endoscopy, unlike the RNY which divides the stomach into an upper and lower pouch, the lower of which cannot be visualized via endoscope.
· DS surgery results in little to no nutritional or metabolic complications as long as the supplementation regime (required for any weight loss surgery) is followed carefully.
· DS surgery results in a superior quality of life to RNY in that patients are able to enjoy eating a normal, balanced diet with no specific food restrictions.
· NO stomal plugging and less vomiting.
Here are some disadvantages of the RNY that your RNY surgeon might not tell you about:
· Sugar is not always the cause of dumping
· Many people don't dump at all
· Many people are vitamin deficient because their food intolerances do not allow them a varied diet
· A lot of RNYers drink meat tenderizer mixed with water because food gets "stuck"
· A huge number of diabetics are not cured by RNY, many improve but not many are cured
· About 68% of those with RNY vomit frequently
· Many people gain at least 50% of the weight back
Lap Band 2/26/03---lost 80 pounds!
FAILED (Erosion/emergency removal) 4/4/07, Gained ALL weight back 8/29/07
Approved for DS 10/09/07 -
DS performed successfully 10/29/07
1st Hernia repair and vertical TT 1/15/09
2nd Hernia repair and small vertical TT 12/27/2010
HW SW CW GW 240 225 159 135 (5ft.2in.)
I had the band and I can totally relate to what you're going through. I was so relieved when it was finally out. I also contenplated RNY until someone pointed me to this forum. It was the best decision I ever made and I love my DS. I wish you the best of luck and suggest you get that device out of your body. It will continue to give you problems down the road. I sure am glad I had it removed.
Valerie
DS 2005
There is room on this earth for all of God's creatures..
next to the mashed potatoes
![]()
 I wrote this on my profile because there is so much about the DS that is beneficial to your health and lifestyle that many don't know about. I want to post it here for you and anyone interested to know what the DS is all about. Yeah... I am known to be extremely detailed oriented when it come to putting my thoughts to print. All those years writing dissertation do that to you, lol.
I wrote this on my profile because there is so much about the DS that is beneficial to your health and lifestyle that many don't know about. I want to post it here for you and anyone interested to know what the DS is all about. Yeah... I am known to be extremely detailed oriented when it come to putting my thoughts to print. All those years writing dissertation do that to you, lol.The DS procedure has been performed since 1988 and combines restrictive and malabsorptive elements to help achieve and maintain longterm weight loss:
1. by restricting the amount of food that can be eaten through a reduction in stomach size
2. limit the amount of food that is absorbed into the body through a rerouting of the intestines
3. have a metabolic effect induced by manipulating intestinal hormones as a result of intestinal rerouting
It is a more involved procedure because it has a significant component of malabsorption and metabolic effect that is achieved by the intestinal bypass effect of the duodenal switch component. The overall effect is that DS patients are able to engage in fairly normal, free eating, while having the benefit of taking on the metabolism of a lean individual.
In RNY procedure, the duodenum and pyloric valve are bypassed and the intestines are connected to a newly created stomach pouch, known as a stoma. This digestive configuration is known as a gastric bypass. The stoma holds one ounce of food, but its exit port is always open and does not store food causing it to glide through into the intestines non-stop which causes a possibility of dumping syndrome. Some consider dumping to be a key component of gastric bypass. Yet, it has been medically proven with published scientific report, data and studies that there is no relation between dumping and weight loss.

With the DS procedure, the duodenum is fully functional with no bypass occurring, since the entry and exit port of the stomach and the pyloric valve are untouched in its digestive configuration and left originally the same way before and after surgery. This allows food and drink to be consumed at the same time and become iso-osmolar during digestion. Keeping food in the stomach until it is digested prevents dumping and provide satiety. This also helps control weight as the DS stomach stretches a bit with time, as it is normally suppose to do. The plyorus stays shut while food and fluid are in the stomach, causing the stomach to work as a hopper and digest the food that provides nutritents as it process, then passes into the doudenum as it continues to absorb nutrients for the body.
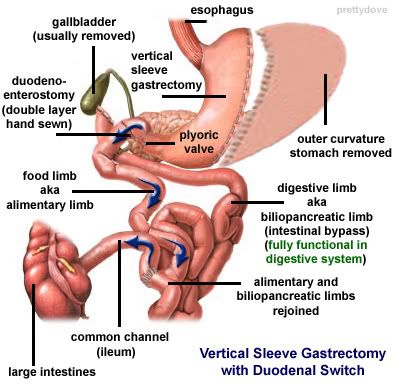
This is important, since, the duodenum is the part of the intestine where protein, calcium, iron and vitamin B12 are absorbed and with the RNY causes these four nutrients to not be absorb. Even though, the DS has a greater malabsorptive factor, it actually has more normal nutritional absorption than the RNY because the duodenum and pylorus are still involved in the digestive process.

As can be observed in the chart above, the DS is able to provide LESS MALABSORPTION of nutrients compared to the RNY, since the stomach and duodenum are left intact and in full functional capacity to process in its digestive system. Therefore, the RNY has more vitamins and mineral malabsorption causing greater possibilities of deficiencies, due to the complete removal (bypass) of the stomach and duodenal from its digestive absorption process.
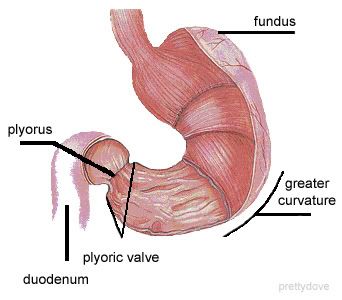
The restrictive part of the DS procedure is known as the vertical sleeve gastrectomy and is achieved via partial gastrectomy (removal of the outer/greater curvature and fundus of stomach). It reduces the size of the stomach 25-30% its original size and into a 2-3cm in diameter tubular structure which holds 3-4 ounces (80-120ml), compared to RNY that holds 15-30ml restriction of food. The grehlin hormone is also removed and eliminates head hunger, cravings and binging from occurring. The sleeve gastrectomy keeps and maintain the pylorus valve intact for the function in the emptying of the stomach contents to the duodenum at its normal controlled pace for better food tolerance and to limit the volume, quantity or amount of food to be eaten.
The malabsorptive component of the DS procedure is the intestinal bypass known as the duodenal switch and achieved by rerouting the small intestine into 2 intestinal tracts known as limbs. One tract separates the flow of food, known as the alimentary limb (or food limb) that measures on average 150-200cm, from the second tract known as the biliopancreatic limb (or digestive limb), where the flow of bile and pancreatic juices comes from the liver and pancreas to process for digestion. Reducing the amount of bile and pancreatic juices the food comes in contact with, reduces the amount of food that is digested and decreases absorption.
The alimentary limb absorbs proteins and sugars from ingested food, secretes the peptide hormone Enteroglucagon or GLP-1, which has 37 amino acids that controls the metabolism of glucose from undigested food.
It suppresses the insulin response when carbs is ingested to reduces the amount that is converted to and stored as fat.
It increases insulin secretion as it decreases glucagon secretion from the pancreas that helps to treat and cure at a rate of 98.9% with PERMANENT REMISSION for Diabetes, even if you regain weight.
Diabetes will not return as per medical research and long-term studies that has been published, documented and recorded in medical journals, with the extremely small and rare exception of 1.1% whose Diabetes was still evident after surgery.
With the RNY, there is a high possibility that weight gain will cause Diabetes to return. It is unlikely with the DS to have post-ops with Diabetes or to have Reactive Hypoglycemia, as proven to occur among those with the RnY or Gastric Bypass surgical procedure (whether at goal or regained weight), after being post-op for over a year or more. For a RNY post-op, reactive hypoglycemia disorder does occur in those who never had Diabetes (related or non-related) prior to surgery or in their life and again is not an occurrence that will happen with post-ops DSers.
The duodenal switch surgical portion has been perform as a stand alone treatment for Diabetes on obese and non-obese patients for over 20 years, based on the mechanics and metabolism process that takes place in the digestive system.
Further down the digestive tract, the two separated limbs of the small intestines are rejoined to be connected at the ileum known as the common channel. This is where the food and digestive juices begin to mix and limit fat absorption, essential for good health to occur. The common channel length varies according to Hess method (100cm) or according to patient's needs, malabsorption level desired, etc., from 50-150cm.
The common channel section is the ONLY portion of the intestines that a DSer is able to absorb calories, fats and complex carbohydrates and no where else in their small intestine digestive system.
With the DS, a person eating food will be able to MALABSORB:
50% of calories
80% of fats
40% of complex carbohydrates
0% of simple carbohydrates
Unlike the Roux-n-Y, the Duodenal Switch is an intestinal bypass and NOT a gastric bypass procedure. It is also a gastric restrictive procedure and again NOT considered a gastric bypass, since, digestion begins in the stomach breaking down food and it keeps the pyloric muscle between stomach and small intestine intact, allowing the stomach contents to start their digestive process before food enters the duodenum. This preservation eliminates the symptoms of dumping syndrome, marginal ulcers, strictures and blockages.
BMI = 23.7 3+ yrs post-op
stomach = 3.5 oz, common channel = 125 cm