
What You Need to Know for the Duodenal Switch (DS)
January 13, 2016As a bariatric surgeon with 20 years of performing weight loss surgery procedures and 10 years performing the Duodenal Switch almost exclusively, I have come to know the pro’s and con’s of the various operations for weight loss. While the type of surgery performed and the way it is performed has changed over the years, many things have remained the same. The patients are still very much the same. They generally consume too many calories, have slower than average metabolisms, and have higher than average hunger drives. Their co-morbidities are also the same. Diabetes, hypertension, hypercholesterolemia fatty liver (NASH), and obstructive sleep apnea are the ones of major concern. These and many more can be cured with weight loss surgery.
The least known, as well as the least performed, of the four major weight loss operations is the Duodenal Switch (DS). None achieve as good of weight loss or co-morbidity resolution as the DS.
I would like to educate you on the things you should know about it so that you can make an informed decision about whether this operation is the right one for you.
What You Need to Know About Body Changes with Duodenal Switch
Patients lose weight after various weight loss operations, either as a result of restriction alone or restriction combined with malabsorption. There are changes in your hormones such as Ghrelin which will reduce your appetite. There may also be changes in your intestinal hormones which can affect how you process the food you eat, and may have an effect on your metabolism. Food choices that limit your calories and exercise to burn more calories also help. In general, you will lose weight and keep it off as a result of eating less calories and/or absorbing only a percentage of what you eat.
I am sure you have heard that these operations are tools to lose weight and you must use these tools properly or else your weight loss may be less than desired. That is true, but probably what was omitted from this talk is that these operations are not equally powerful in helping you achieve your goal.
By far, the most powerful operation is the DS.
And as a result of the DS's power, the long term (10-year post op) excess weight loss (EWL) is about 75%. This has been shown in several different peer reviewed studies. This contrasts significantly with studies of EWL for the other three operations (Roux-en-y gastric bypass (GB), Sleeve Gastrectomy (SG), and the Laparoscopic Adjustable Gastric Band (LAGB) where there is probably no good long term study of 10 years or more. Even the shorter term studies show excess weight loss in the 60% to 65% range.
If we define “success for weight loss after bariatric surgery as 50% EWL at 5 years”, many procedures are not making this success mark. More importantly, the number of people with a Body Mass Index (BMI) which is still morbidly obese can be as high as 25%-30% with the GB or SG. With the LAGB, that number is far higher. With the DS it is far less!
With the increased power of the DS comes with increased responsibilities. Because the DS both limits your food intake and creates more significant malabsorption, you have a need to be a responsible weight loss surgical patient. Taking your vitamins and supplemental protein is mandatory. Following up with your bariatric surgeon yearly to get your malabsorptive blood panel is equally important.
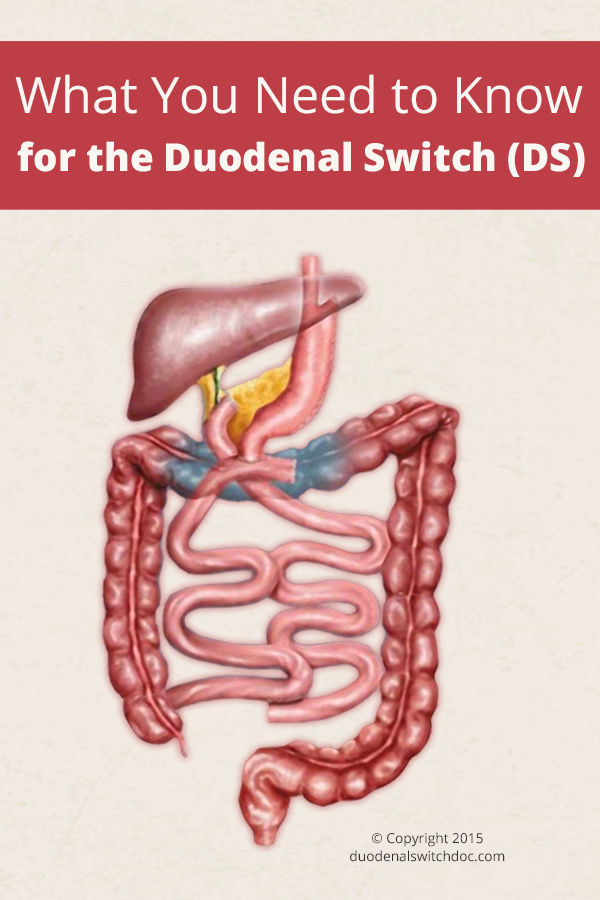
Anatomy of Duodenal Switch
The altered anatomy of a DS is fairly unique. The stomach is made into a narrow tube or sleeve. The diameter of that tube may vary and the last part of that tube can be a little wider. Originally the size of this tube would hold about four ounces but as the SG evolved, the volume of this new stomach has become even more restrictive. The DS has generally maintained a larger volume than the purely restrictive SG but there is a trend to make this volume more restrictive and lengthen the common channel, thereby reducing the mal-absorptive part of the operation.
The malabsorptive part is created by transecting the duodenum (very beginning of the intestine) and creating a Roux-en-y hook up with a long limb for the bile salts and pancreatic enzymes, and a shorter limb for the food passage. These two limbs then come together forming the common channel where most of the absorption occurs.
Vitamin and Protein Needs for Duodenal Switch Patients
All DS patients need to take vitamins on a daily basis, starting with a good multivitamin. It should have all of the FDA requirements but in addition, it should have extra Vitamin A, D, E, and K. These are the fat soluble vitamins. They require the presence of bile mixing with these vitamins for absorption. Since your food, these vitamins and your bile salts spend a reduced amount of time together in the GI tract, you require increased amounts of these vitamins to maintain normal vitamin levels. Checking these levels with periodic blood tests and adjusting what you take is important.
Iron is poorly absorbed in DS patients and varying amounts of iron should be taken. Menstruating women, in particular, need extra iron. Iron deficiency anemia will result if ignored.
Extra calcium in the form of citrate (not carbonate) may be required in doses of about 2400 mg per day. If you do not take enough calcium, you can gradually get softening of your bones (osteoporosis).
Your B vitamins, in particular B1 and B12, should be additionally taken and these levels monitored.
Lastly, as your total intake is limited and your absorption is reduced, you need to pay extra special attention to your protein intake. Water intake is number 1. Protein intake is number 2. After consuming adequate protein amounts (80-100+ grams per day depending on your size and activity level), you can then consume everything else. Vegetables and fruits for fiber should also be included. Normal eating is one of the best benefits of the DS and patients enjoy eating meat and nuts as a good protein source. Protein supplements can help as well if needed. If you do not maintain your protein level you can become very sick with generalized weakness and swollen legs.
Side Effects of Duodenal Switch
Loose bowel movements and excess flatus can accompany the DS. Because you don’t absorb fat normally, the unabsorbed fat which enters the large intestine causes you to have looser bowel movements and possibly diarrhea. Typically DS patients will have a fairly large bowel movement in the morning followed by a small looser bowel movement within the hour. They then proceed throughout the remainder of the day and have another soft bowel movement in the evening.
You also don’t absorb complex carbohydrates normally. Simple carbs (sugar, fruit juices, flour) are easily absorbed. Some of the complex carbs may proceed into the large intestine. The billions of bacteria in your large intestine will then metabolize these carbohydrates and produce gas as a byproduct, giving you more gas to expel.
These side effects can be non-existent, mild, or more severe depending on your diet. The potential for these can be discussed before your surgery and steps taken to prevent them. Lengthening your common channel will increase your ability to absorb a higher percentage of the fat and carbohydrates in your diet and limit these side effects. It will also mildly reduce your weight loss. This can be countered by making the stomach part of the operation a little more restrictive thereby maintaining your weight loss
Is the Duodenal Switch Right for You?
The DS is an appropriate weight loss operation for anyone who meets the criteria for any bariatric surgery. There are however, two types of people who would specifically benefit from this more aggressive operation. One is the super morbidly obese patient with a BMI over 50. These patients more commonly do not lose enough weight with other weight loss operations and as a result are unsatisfied with their eventual weight. Those with a metabolic syndrome would also benefit significantly. They typically have diabetes, hypertension, and hypercholesterolemia of varying degrees of severity. Even though they may not have a very high BMI, the more powerful operation is very helpful in eliminating their co-morbidities and maintaining their long term health better than the other operations.
Lastly, there are a large number of patients who have undergone one of the other operations with less than satisfying results or serious side effects. Conversion to a DS is certainly an option but one which must be tempered with an even higher surgical risk. That is why choosing the proper weight loss operation for you the first time is by far the best. Avoiding revision surgery for any reason is certainly preferred.
Choosing a weight loss operation is certainly more difficult than it was 20 years ago. Understanding the pro’s and con’s of each and how it will affect you is the best way to make that decision. Choosing a surgeon is also very important as he/she can guide you in making this decision. Having a surgeon with sufficient knowledge of all of the options and experience in performing them would be optimal.
 | ABOUT THE AUTHOR David F. Greenbaum, MD, FACS is the past director at LMCBC and currently at Virtua Health Systems, Virtua Memorial Hospital in Mt Holly, NJ. Dr. Greenbaum is a member of the American Society for Metabolic and Bariatric Surgery (ASMBS), a past chairman of the Public and Professional Committee and a member of several other committees at the ASMBS.Read more articles from Dr. Greenbaum! |



