
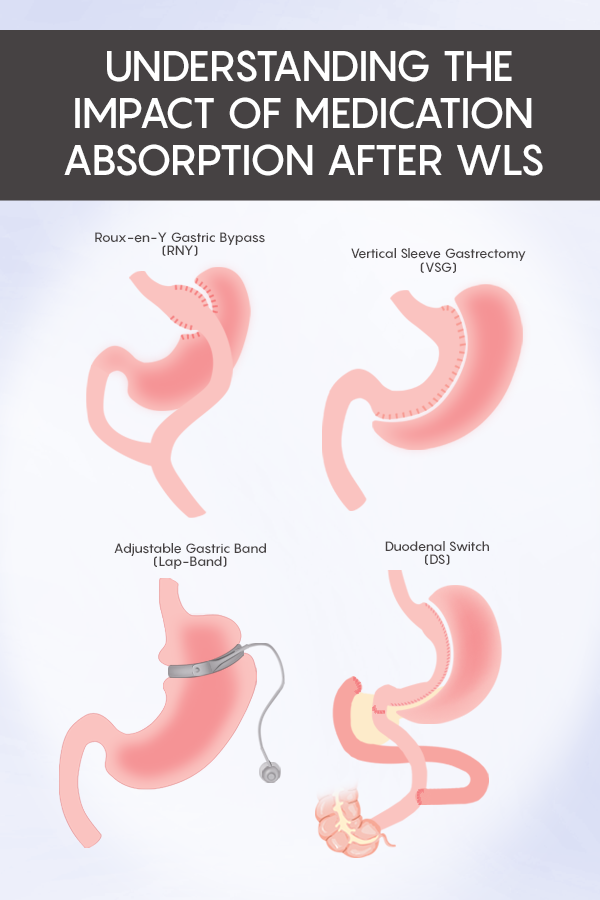
Understanding the Impact of Medication Absorption After WLS
January 27, 2020Patients undergoing weight loss surgery are usually on one or more medications, and the medication absorption after WLS may change. There are several factors that will affect the absorption of your medications after weight loss surgery. The two main determinants of absorption depend on the medication and the procedure you had.
Medication Absorption in Post-Operative Phase
In the immediate post-operative phase, most surgeons will change tablets to a liquid/elixir formulation, if available. Otherwise, you may be asked to break them if they are large. If that is not possible, they may be switched from long-acting for the shorter-acting version to allow better control and prediction of their absorption. It’s vital to let your surgeon know what are the medications you are on as well as how long you have been on each of them.
Breaking tablets into smaller fragments is generally not recommended as this will affect their absorption rate and pharmacokinetic (they way medications interact with your body once ingested). Many medications are made into long-acting formulas, so they aren’t easily absorbed when they meet the acidic conditions of the stomach.
Let’s take hypertension medications as an example. Many bariatric patients are on one or more anti-hypertensives before having weight loss surgery. If you have been on anti-hypertensive medications for an extended period of time, it’s strongly advised not to stop them abruptly. However, if you break long-acting formulations, it will be absorbed very rapidly, causing a sudden drop in blood pressure. You may feel light-headed and/or even pass-out if the blood pressure drops too low.
Furthermore, the medication may not last as long in your system because it was absorbed very rapidly which means you may have rebound hypertension. In this instance taking your medication may cause significant harm.
Many other medications may not be stopped abruptly as one risks having severe side effects secondary to abrupt cessation of these medications. A few examples include, but are not limited to, diabetes medications, psychoactive medications, certain analgesics, and anxiolytics. Stopping these mediations suddenly will result in serious adverse effects; in fact, they may cause life-threatening situations.
I am going to discuss the changes which occur after four common procedures and how each may affect medication absorption.
PLEASE BEWARE this is for EDUCATIONAL purposes so you can discuss the matter with your physicians, I STRONGLY ADVISE YOU AGAINST making these decisions unilaterally.
Vertical Sleeve Gastrectomy (VSG)
The surgeon will remove a portion of the stomach during this operation. The parts of the stomach removed are fundus, body, and a portion of the antrum. After this procedure, there are both anatomical and physiologic changes. To start with, your stomach is about 75% smaller and shaped into the letter ‘J.’ The tubular stomach will empty faster than prior to surgery, and it will lack some of the hormonal activities which it had prior as well since some portions of the stomach are removed.
Most surgeons will ask you not to take large pills immediately after this procedure. In my practice, I use a 36 French Bougie to create the new stomach, which means the upper part of the stomach is about 1.5 cm in diameter, that’s 1/2 an inch. Immediately after the surgery, there will be some inflammation of the stomach lining, making this diameter even smaller.
So, I will make some modifications to your medications depending on what they are, large tablets can get stuck in the upper parts of the sleeve, and that can cause nausea with violent vomiting. This may also lead to other more severe complications such as staple line disruption, which will manifest as a leak, one of the most serious complications of any stapling procedure, and this will be life-threatening!
Roux-En-Y Gastric Bypass (RYGB, RNY)
The new anatomy in this procedure consists of a stomach pouch, which is the size of a medium egg, about 30 cc in size, and a connection between the stomach and the small bowel the size of your pinky tip. You can imagine what will happen if you try to force a large tablet through that. You will risk obstruction, and suture disruption, as mentioned above, will lead to a life-threatening condition.
RYGB is also unique in that it allows for a shortcut in absorption since about 150 cm of the small bowel is bypassed altogether. This means medications will spend a much shorter time in the stomach and the small intestine. The effect of this change depends on the medication, and some formulations will get absorbed faster, whereas others may not have time to get absorbed entirely so they may not be absorbed effectively.
In the former situation, the medication dosage may need to be reduced, whereas in the later, the dosage needs to be increased, or the formulation needs to be changed to liquid/capsule depending on the timing after surgery and availability of other formulas.
Biliopancreatic Diversion / Duodenal Switch (DS)
While these two procedures are slightly different, their effect on medications is very similar to the Roux-En-Y gastric bypass. However, since more of the small intestine iOS bypassed in both of these procedures, their impact on certain medications will be even more exaggerated than the Roux-En-Y gastric bypass.
Adjustable Gastric Band (Lap-Band)
The band doesn’t change the anatomy of the gastrointestinal tract, but it’s a rigid ring that is placed at the entrance of the stomach. If your medications are large, the tablets may not be able to get to the stomach and will not get absorbed for it to work. If you have diabetes and hypertension, for example, it may be worthwhile to discuss the procedure you had done with all your providers as you may need further investigation to ensure the medications are absorbed as intended.
As there are many anatomical, physiological, and hormonal changes after weight loss surgery, you must discuss with your bariatric surgeon how to resume these medications after surgery.
 | ABOUT THE AUTHOR Dr. Husain Abbas of Memorial Advanced Surgery, is a Board Certified surgeon trained in Minimally Invasive Surgery. After his surgical residency at St. Mary's, a Yale University affiliated hospital, Dr. Abbas completed a fellowship in Minimally Invasive Gastroesophageal & Bariatric Surgery at the University of Florida, Gainesville. Dr. Abbas' expertise extends to a wide array of gastroesophageal disorders, anti-reflux surgery, complex hernia repairs, endocrine, oncology and bariatric procedures.Read more articles from Dr. Abbas! |



